U.S. Maternal Mortality
A look at U.S. health outcomes

“84% of pregnancy-related deaths are preventable”
(The CDC, 2021)
Overview
Maternal mortality is defined as a pregnancy-related death that occurs while pregnant or within one year of the end of pregnancy from any cause related to or aggravated by the pregnancy (PMSS, n.d.).
Pregnancy-related deaths varied in timing:
- 22% of deaths occurred during pregnancy
- 25% occurred on the day of delivery or within 7 days
- 53% occurred between 7 days to 1 year after pregnancy (CDC, 2022).
Data Disclaimer
A lack of standardized methods and terminology for identifying maternal deaths in the United States has resulted in nuanced data collection and interpretation challenges (Collier & Molina, 2020).
Although these challenges continue to exist in the data collection process, current data trends still show a steady increase in U.S. maternal mortality and morbidity.
Many factors influence the U.S. maternal mortality rate. These include both clinical factors and social determinants of health. The rise of chronic health conditions has also exacerbated patient outcomes during pregnancy. Additional information on these factors will be discussed in the later sections.

A Global Perspective: How Does the U.S. Compare to Other OECD Countries?
The OECD defines healthcare expenditure as the final consumption of healthcare goods and services. This includes personal health and collective services. Since the 1970s, the United States has consistently spent the most on health expenditures (OECD, 2024).
"Globally, maternal mortality has decreased 43 percent since 1990; the United States is the only developed country where it has gone up"
Compared to other industrialized high-income countries, the U.S. has the highest rate of maternal mortality. Since the COVID-19 pandemic exacerbated barriers to care, transportation, employment, and mental health resources, maternal mortality has worsened since the pandemic (Simpson, 2023).

Maternal Outcomes Vary by Race
In the U.S. maternal mortality continues to disproportionately affect women of color. 2021 Data from the CDC portrays the disparities among race and maternal outcomes. The data excludes 2021 data for Asian mothers.
Compared with white women, black women were more likely to report:
- Being treated unfairly and with disrespect by providers because of their race
- Not having decision autonomy during labor and delivery
- Feeling pressured to have a cesarean section (Declercq & Zephyrin, 20220).
" Black women are more likely than white women to report that their concerns and preferences regarding birth were disregarded "
What Conditions Cause Maternal Mortality?
There are many underlying causes of maternal death:
- Chronic medical conditions (cardiovascular conditions, hemorrhage, etc.)
- Unintentional death from violence, overdose, and self-harm
- Existing inequities in pregnancy care (Collier & Molina, 2020).

Examining The Issue In-Depth

A Look Into the Maternal Care Workforce
There is a concerning number of maternity care deserts that lack access to obstetric hospitals, centers, and providers. A report published by March of Dimes found that 36% of U.S. counties (largely in the Midwest & South) lack resources for pregnant families. Women and infants in maternal care deserts face higher risks of poor health outcomes and preventable death (Treisman, 2022).
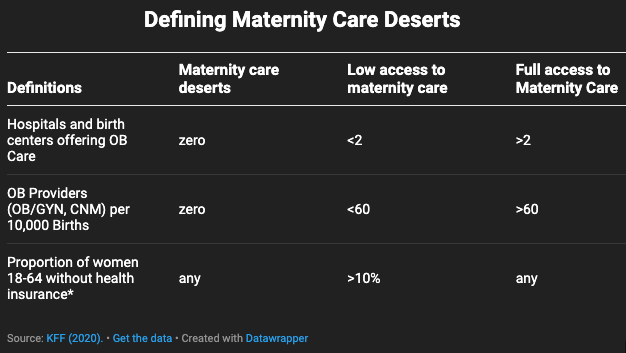
What is a Maternal Care Desert?
A majority of maternal care deserts are in rural communities. The criteria for defining accessibility to OBGYN services are defined below.
Mistreatment During Pregnancy:
- 1 in 5 women reported mistreatment while receiving maternity care
- 1 in 3 women of color reported mistreatment
- 45% of women held back from asking questions or sharing concerns during their maternity care (CDC Vital Signs, 2023).
Importance of Prenatal Care
Early and regular prenatal care improves the chances of a healthy pregnancy
During a prenatal visit, a provider will make recommendations to promote a healthy pregnancy and birth:
- Take steps to manage existing medical conditions
- Provide additional resources and advice
- Increasing folic acid intake - provides a 70% reduction in the risk of neural tube defects (Kabella, 2023).
Paid Maternity Leave
While some states have opted to provide paid family or medical leave, there is no federal law that mandates this. The lack of paid maternity leave subjects families to harmful time and financial constraints.
Paid parental leave has been attributed to:
- decreased infant mortality,
- decreased rehospitalization rates
- lower risk for post-partum depression
- improved child development
- increased income over time (ACOG, 2023)
The U.S. is the only high income country in the world that doesn't have a national paid family leave (PFL) policy.

The High Cost of Childbirth
Compared with women with private health insurance, women with Medicaid coverage were more likely to report:
- No postpartum visit
- Returning to work within two months of birth
- Less postpartum emotional and practical support at home
- Not having decision autonomy during labor and delivery
- Being treated unfairly and with disrespect by providers because of their insurance status (CommonWealth, 2020).
Similar to race, women's experience with the health care system varied by insurance coverage. As a result, patient outcomes also differ across income, location, and insurance status.

Impact on U.S. Families
Maternal death implies long-term economic and social repercussions for the families they leave behind.
- In 2019, 41.2% of mothers were the sole breadwinners for their families (Glynn, 2021)
- Increased mortality risk for children 0 to 9
- Decreased nutrition and schooling for children
- Higher rates of poverty
- Lack of household resources and management (National Research Council (US) Committee on Population, 2000)
The U.S. healthcare system needs to reconsider how to address this problem. Disparities in patient care influence outcomes across race, income, gender, & geography.
A country that spends the most on health care has the resources to create a more efficient and equitable system. Ultimately, mitigating barriers to care and expanding accessibility are key to improving health equity.


Photo by Kelly Sikkema on Unsplash
Photo by Kelly Sikkema on Unsplash

Photo by Juan Encalada on Unsplash
Photo by Juan Encalada on Unsplash

Photo by Craig Pattenaude on Unsplash
Photo by Craig Pattenaude on Unsplash

Photo by Bonnie Kittle on Unsplash
Photo by Bonnie Kittle on Unsplash

Photo by Andrae Ricketts on Unsplash
Photo by Andrae Ricketts on Unsplash

Photo by Christian Bowen on Unsplash
Photo by Christian Bowen on Unsplash
Supporting U.S. Mothers

Potential Interventions
Key interventions to improve maternal health outcomes:

Photo by March of Dimes on marchofdimes.org
Photo by March of Dimes on marchofdimes.org
Addressing Maternal Care Deserts
- Expand care by utilizing a mobile clinic.
- Pilot programs launched in D.C. and Ohio have found success with mobile clinics in high-need areas (Marchofdimes 2022).
- Encourage the use of telehealth for patients who cannot make an in-person visit to their provider.
- Increase the prevalence of maternal health workers in rural areas by offering loan forgiveness or grants.
- Existing incentives such as the NHSC Loan Repayment Program can expand their criteria to offer loan forgiveness in exchange for service in rural care deserts (NHSC, 2023).

Photo by charlesdeluvio on Unsplash
Photo by charlesdeluvio on Unsplash
Mandated Parental Leave
- Implementing a federally mandated paid leave for new parents supports better economic and health outcomes for both the mother and child.
- In place of a current federal mandate, states can elect to pass individual policies to protect family leave as a medical right.
- The American College of Obstetricians and Gynecologists advises at least 8 weeks of paid leave are needed (ACOG, 2023).

Photo by Volodymyr Hryshchenko on Unsplash
Photo by Volodymyr Hryshchenko on Unsplash
Managing Risk Factors
- Early access to adequate prenatal and postpartum care can mitigate pregnancy risks and death.
- Passing a Medicaid expansion on postpartum services from 60 days to 12 months can ensure mothers and babies are supported during this critical period.
- Given that more than half of pregnancy-related deaths occur during the year following delivery, it's critically important to expand postpartum care (Katon, et al., 2021).
Stay Informed!

Addressing Change:
To stay informed on the latest news or issues regarding maternal health please volunteer or advocate using the links below:
Resources:
- March of Dimes is a great non-profit that focuses on improving the health outcomes of moms and babies.
- The link below connects you with various resources, programs, events, and initiatives.
References
Breadwinning Mothers Are Critical to Families’ Economic Security. (2021, March 29). Center for American Progress. https://www.americanprogress.org/article/breadwinning-mothers-critical-familys-economic-security/
CDC. (2023, September 29). Mistreatment during maternity care. Centers for Disease Control and Prevention. https://www.cdc.gov/vitalsigns/respectful-maternity-care/index.html
CDC Newsroom. (2016, January 1). CDC. https://www.cdc.gov/media/releases/2022/p0919-pregnancy-related-deaths.html
Collier, A. Y., & Molina, R. L. (2019). Maternal Mortality in the United States: Updates on Trends, Causes, and Solutions. NeoReviews, 20(10), e561–e574. https://doi.org/10.1542/neo.20-10-e561
Easing the Burden: Why Paid Family Leave Policies are Gaining Steam | Stanford Institute for Economic Policy Research (SIEPR). (n.d.). Retrieved February 27, 2024, from https://siepr.stanford.edu/publications/policy-brief/easing-burden-why-paid-family-leave-policies-are-gaining-steam
Health resources—Health spending—OECD Data. (n.d.). theOECD. Retrieved February 11, 2024, from http://data.oecd.org/healthres/health-spending.htm
Health Status: Maternal and infant mortality. (n.d.). Retrieved February 11, 2024, from https://stats.oecd.org/index.aspx?queryid=30116
Hill, L., Artiga, S., & Published, U. R. (2022, November 1). Racial Disparities in Maternal and Infant Health: Current Status and Efforts to Address Them. KFF. https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-in-maternal-and-infant-health-current-status-and-efforts-to-address-them/
Home. (n.d.). Peterson-KFF Health System Tracker. Retrieved February 12, 2024, from https://www.healthsystemtracker.org/
How Much Does It Cost To Have A Baby? 2024 Averages – Forbes Advisor. (n.d.). Retrieved February 11, 2024, from https://www.forbes.com/advisor/health-insurance/average-childbirth-cost/
Inadequate prenatal care: United States, 2017-2022. (n.d.). March of Dimes | PeriStats. Retrieved February 11, 2024, from https://www.marchofdimes.org/peristats/data?reg=99&top=5&stop=34&lev=1&slev=4&obj=1
Length of paid leave (calendar days). (n.d.). World Bank Gender Data Portal. Retrieved February 11, 2024, from https://genderdata.worldbank.org/indicators/sh-leve/
Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries. (2020, November 18). https://doi.org/10.26099/411v-9255
Maternal Mortality in the United States: A Primer. (2020, December 16). https://doi.org/10.26099/ta1q-mw24
Maternal Mortality Is on the Rise: 8 Things To Know. (n.d.). Yale Medicine. Retrieved February 11, 2024, from https://www.yalemedicine.org/news/maternal-mortality-on-the-rise
Maternal Mortality Rates in the United States, 2021. (2023, March 16). https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm
NHSC Loan Repayment Program | NHSC. (n.d.). Retrieved February 27, 2024, from https://nhsc.hrsa.gov/loan-repayment/nhsc-loan-repayment-program
Population, N. R. C. (US) C. on, Reed, H. E., Koblinsky, M. A., & Mosley, W. H. (2000). EVIDENCE ON THE CONSEQUENCES OF MATERNAL MORTALITY. In The Consequences of Maternal Morbidity and Maternal Mortality: Report of a Workshop. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK225436/
Pregnancy Mortality Surveillance System | Maternal and Infant Health | CDC. (2023, March 31). https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm
Simpson, K. R. (2023). Effect of the COVID-19 Pandemic on Maternal Health in the United States. Mcn. the American Journal of Maternal Child Nursing, 48(2), 61. https://doi.org/10.1097/NMC.0000000000000895
The U.S. Maternal Mortality Crisis Continues to Worsen: An International Comparison. (2022, December 1). https://doi.org/10.26099/8vem-fc65
Treisman, R. (2022, October 12). Millions of Americans are losing access to maternal care. Here’s what can be done. NPR. https://www.npr.org/2022/10/12/1128335563/maternity-care-deserts-march-of-dimes-report
U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes. (2023, January 31). https://doi.org/10.26099/8ejy-yc74
What Explains the United States’ Dismal Maternal Mortality Rates? | Wilson Center. (n.d.). Retrieved February 20, 2024, from https://www.wilsoncenter.org/event/what-explains-the-united-states-dismal-maternal-mortality-rates
Working Together to Reduce Black Maternal Mortality | Health Equity Features | CDC. (2024, January 8). https://www.cdc.gov/healthequity/features/maternal-mortality/index.html
World Bank Gender Data Portal. (n.d.). World Bank Gender Data Portal. Retrieved February 12, 2024, from https://genderdata.worldbank.org/
