Strengthening Digital Infrastructure and Telehealth Capabilities for a Healthier Rural America

Facing lower life expectancy, higher rates of chronic diseases, and worse outcomes for treatable conditions, rural communities experience persistent health disparities. However, the low number of providers and limited health infrastructure in rural areas make it difficult for many people living in rural areas to consistently access healthcare with traditional in-person methods. With signals that travel miles in an instant, telehealth has the potential to link people in rural area to crucial healthcare resources. Though many rural communities express interest in telehealth, limited digital infrastructure and limited resources to support providers often stymies the implementation of sustainable telehealth programs in rural areas.
You can Support Telehealth in Your Community
Every member of your community deserves access to healthcare, and telehealth has the potential to connect your residents with crucial health resources that they struggle to access. However, implementing sustainable, accessible, and easy-to-use telehealth systems in your community can be challenging. For telehealth to successfully take root in your community, it needs to be accepted and utilized by both providers and community members. By determining the challenges your community is facing and learning about actionable strategies to address these problems, you can build the foundation for high-quality, sustainable telehealth in your community.
As this article explores the experiences of rural providers and community members from a population perspective, you can gain a better understanding of your community's story. Throughout this narrative, callouts will remind you to reflect on your community's experiences as this article prepares you to develop a telehealth strategy specific to your unique community.
Disparate Outcomes and High Rates of Risk Factors Characterize Rural Health

Over 57 million Americans live in rural areas that are characterized by persistent health disparities. Compared to urban areas, rural populations experience much higher rates of many chronic diseases including diabetes, COPD, high blood pressure, and arthritis. Chronic diseases are 'leading cause of death and disability in the United States' according to the Partnership to Fight Chronic Disease. Each of these conditions requires ongoing care and management over long periods of time, which means continuity of care is especially important. In addition to experiencing particularly high rates of chronic diseases, rural populations have the higher mortality rates for the five leading causes of death, several of which are the result of chronic diseases.
The combination of higher mortality rates for many of the leading causes of death results in rural areas having a lower life expectancy, and researchers have found that the rural-urban life expectancy disparity has been growing steadily over the past two decades. A CDC study found that a large percentage of these deaths were preventable, which indicates need for public health intervention to address factors that contribute to preventable disease and death.
Rural populations have higher rates of many risk factors associated with increased risk for chronic diseases like diabetes, heart disease, high blood pressure, and stroke. While cross-sectoral social policy plays an important role in addressing social and environmental contributors in preventing these outcomes, access to healthcare is key to ameliorating some of these disparities through improving health education and facilitating health behavior change.
From improving health literacy to delivering preventative care to managing chronic diseases, healthcare professionals provide essential services to keep populations healthy. Regular contact with trained healthcare professionals, such as doctors, nurses, and therapists, provides opportunities for people to live longer, healthier lives. The need for medical practitioners in rural communities is clear, but, unfortunately, rural populations tend to face many barriers to accessing healthcare.
What health conditions have the greatest impact on your community?
What health risk factors are prevalent in your community?
Healthcare Access Remains Out of Reach for Rural Americans

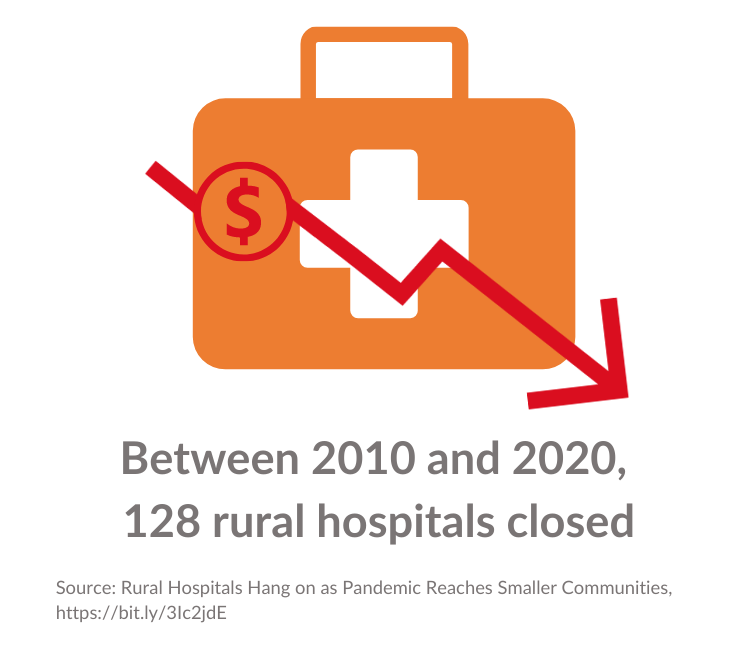
Rural Health Facilities Struggle Under the Weight of Financial Challenges
Low numbers of healthcare facilities and healthcare providers pose challenges to healthcare access in rural communities. Healthcare facilities, particularly hospitals, tend to face more financial difficulties than their urban counterparts. High rates of closures among rural hospitals have made it more difficult for rural populations to access specialty and emergency care.
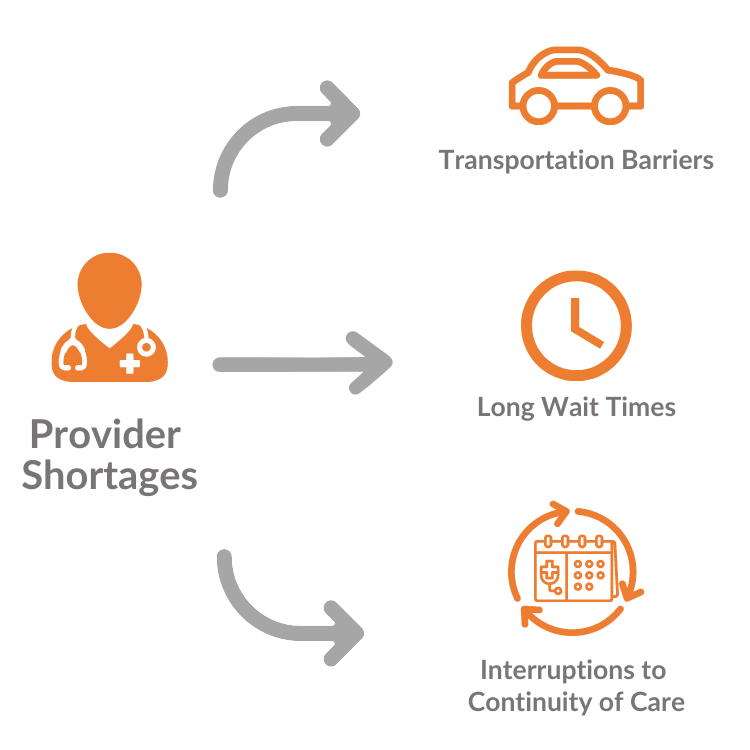
Severe Provider Shortages Persist
The low-density distribution of healthcare providers also reduces the accessibility of healthcare for people living in rural areas. While approximately 17% of the population lives in rural areas, under 8% of doctors practice in these areas. When assessing the number of providers per 10,000 population, rural counties consistently have lower ratios of providers than urban counties for all doctors, primary care physicians (PCPs), and dentists. While efforts have been made to increase the number of physicians practicing in rural areas with programs like loan forgiveness, the number of providers in rural areas has continued to shrink.
Patients Struggle to Overcome Distance to Health Resources
The limited availability of healthcare facilities and providers builds to another barrier to access: distance. Since rural areas are less densely populated than urban areas, people in rural areas tend to travel longer distances to their medical providers. As the number of providers and health facilities shrinks, the distance to the nearest provider grows for many members of the community. Long distances impose time and transportation constraints on patients who may have to take off several hours of work to get to one appointment. This is especially problematic for patients with chronic diseases who may need regularly scheduled appointments to consistently manage their condition. As the amount of time required to travel to an appointment increases, the feasibility of attending reoccurring appointments decreases for individuals who cannot afford to take off the required number of work hours or have other obligations that prevent them from leaving home for long periods of time.
What, if any, health facilities are located in your community? Nearby communities?
How far away is the nearest hospital?
Do any health practitioners live in your community?
What health services do people in your community have the greatest need for?
What types of providers are the most inaccessible to community members?
Telehealth is an Opportunity to Expand Access


Telehealth is particularly well-suited to address many of the factors that reduce access to healthcare in rural areas. By providing a virtual platform for linking to providers outside the immediate area, people are able to reach specialists and other providers that are not practicing in rural areas. Virtual appointments also reduce distance barriers as patients no longer need to use time consuming transportation to get to appointments with providers in rural areas. By making providers both inside and outside the immediate area more accessible via virtual appointments, it becomes easier for patients to schedule regular appointments, which supports the continuity of care for chronic diseases. Lastly, research has found that when implemented effectively, telehealth can provide economic benefits to rural communities by improving the utilization of healthcare services in rural areas and thereby improving the financial viability of rural healthcare practices.
While there are clear benefits to utilizing telehealth in rural areas, the adoption and usage of telehealth still lag in rural areas. Poor digital infrastructure and limited resources to support provider implementation of telehealth have hindered its expansion in rural areas.
The Digital Divide Remains a Barrier to Telehealth Expansion

The digital divide describes the unequal distribution of digital resources, including broadband, personal devices, and knowledge, between rural and urban populations. Though each of these three components of the digital divide poses challenges to the implementation of sustainable telehealth, access to high-speed broadband is the foremost factor necessary for a successful telehealth system. Two of the primary forms of telehealth are video appointments and remote data collection via at-home medical equipment. Both of these processes require connection to steady, high-speed broadband. Unfortunately, there are low rates of broadband availability in rural counties, and the median broadband speed available in many rural counties does not meet the traditional definition of high-speed broadband, which calls for speeds of 25 MBPS or greater.
Though significant progress has been made in helping rural counties achieve the high-speed broadband standard as of 2021, the bipartisan group of congressmen leading the Broadband Caucus have called on the FCC to increase the classification of high-speed broadband to 100 MBPS to fit the needs of current technology, which tends to have higher broadband demands than the technology available when the original classification was developed. Under this new proposed standard, very few rural counties would have median broadband speeds that achieved high-broadband speed. In other words, in the vast majority of rural counties, under half of the population would have access to high-speed broadband.
In addition to having lower access to broadband, rural populations tend to own less internet capable personal devices and possess less knowledge relevant to utilizing telehealth. People living in rural areas are less likely to own personal computers and tablets, two key resources utilized for telehealth video conferencing. Additionally, a higher percent of people in rural areas report never utilizing the internet. Lack of internet usage coupled with lack of personal devices results in low levels of digital literacy, meaning low levels of knowledge about the use of common digital tools. When low digital literacy is combined with the low levels of health literacy found in rural areas, the result is low digital health literacy. Digital health literacy describes the ability to navigate online resources and tools for health purposes, and low levels of digital health literacy makes it difficult for people to utilize telehealth tools even if they have access to personal devices and broadband.
What is the median broadband speed in your county?
Who are the primary internet service provider(s) in your community?
Are there any groups in your community that likely have low digital literacy?
Providers are Slow to Adopt Telehealth as They Worry About Support and Sustainability

Providers in rural areas have been slower to adopt telehealth resources and still tend to use them at lower rates than their urban counterparts. A survey conducted on providers currently using telehealth during the COVID-19 pandemic found that many rural providers had only recently begun utilizing telehealth services in their practices whereas many urban providers tended to have incorporated telehealth into their practices earlier.
This survey also assessed provider concerns about continuing to utilize telehealth after the COVID-19 pandemic. Overall, rural providers had higher levels of concern than urban providers. The only potential barriers for which urban providers expressed more concern were liability and licensure, which are both components that become relevant after a facility has determined that telehealth is a feasible option. Rural providers had much higher concerns about the sustainability of a telehealth system after COVID-19, with particularly high rates of concern the cost of maintaining telehealth, the need to continue implementing new technologies, and low patient engagement.
Rural clinics tend to be relatively small and the purchase and implementation of telehealth systems is a costly and resource intensive commitment. Additionally, since many rural clinics already experience financial difficulties, the limitations on reimbursement for telehealth services slowed the implementation of telehealth. During COVID-19 temporary reimbursement parity was established for many services delivered via telehealth, but rural providers still cite concerns over reimbursement and the financial sustainability of telehealth after those temporary regulations expire.
Do any providers in your community or in nearby communities offer any telehealth services? If so, what kind?
What is the technical capacity of your local health providers?
What electronic medical record systems do nearby providers use?
Current Policies Make Strides,
But Gaps Remain

Policies Addressing the Digital Divide
Over the past two years, the federal government has implemented two programs that work to overcome the digital divide by improving access to digital resources.
The Rural Digital Opportunity Fund: An FCC program that will provide 20.4 billion dollars in funding over the next 10 years to build broadband infrastructure for an estimated 5.2 million people. While the program only requires service providers to provide 25 MBPS, the winning bids largely committed to provide communities with speeds of 100 MBPS, which matches the new proposed standard for high-speed broadband.
The Emergency Broadband Benefit Program: Initially legislated for the duration of COVID-19, the program addresses the affordability of broadband and personal devices, the FCC is currently receiving comments for a new, extended version of the program that will be known as the Affordable Connectivity Program. Though neither the current program nor its proposed replacement specifically target people living in rural areas, they both provide financial assistance toward the purchase of broadband and certain personal devices for people with low incomes. Since rural populations tend to have lower median income, this policy can help make broadband and personal devices more affordable for rural Americans. The specific monetary benefits vary depending on the eligibility requirements met by enrollees and are expected to change upon initiation of the new program.
Challenges to Overcoming the Digital Divide Remain:
- While the Rural Digital Opportunity Fund will provide broadband to some rural Americans, not all underserved rural communities will receive broadband through the program
- Recent research indicates that the FCC has overestimated the availability of broadband, particularly in rural areas, and these biased estimates may result in some communities not being identified for appropriate programs
- Community members may lack knowledge of the Emergency Broadband Benefit Program
- Neither of these programs work to improve digital literacy
Policies Supporting Provider Adoption of Telehealth Services
Two recent efforts have helped provide medical practitioners with resources to support the development, implementation, and maintenance of telehealth systems.
Distance Learning and Telemedicine Grants: These grants provide funding for health systems in digitally underserved to acquire video conferencing equipment and software, which can offset the initial costs of implementing a telehealth system. Additionally, these grants can be used to fund infrastructure to connect health systems to higher quality broadband infrastructure, which can enable rural health systems to operate more extensive telehealth systems.
New Telehealth Legislation in the Wake of the COVID-19 Pandemic: For many years, regulations for telehealth developed much more slowly than the technology. The lack of regulation and reimbursement rules made telehealth a risky and financially less profitable service for many years. Throughout COVID-19, efforts to implement social distancing and keep health facilities open for COVID-19 patients resulted in extensive new regulations that offered legal protections to providers and established financially amenable reimbursement for many services. Several examples of COVID-19 concurrent telehealth regulation are provided below.
- Flexible HIPAA requirements to alleviate legal risks for utilizing video conferencing technology
- Telehealth waivers that provide expanded reimbursement for many Medicaid and Medicare services provided via telehealth
- Allowing private insurers to modify benefits mid-year if expanding telehealth coverage
- Allow for the intake of new patients via telehealth
- Allow for the initiation and continuous prescribing of medication assisted treatment for opioid use disorder
- Increased flexibility for practicing telehealth across state lines
Challenges to Provider Adoption of Telehealth Remain:
- Many local providers may not be aware of the Distance Learning and Telemedicine Grants
- Providers may lack the staff or resources to continuously manage a telehealth program
- Many of the regulations that were initiated during COVID-19 have not been made permanent and may eventually expire, which could contribute to provider concerns about the sustainability of telehealth after COVID-19


Has your community been selected for any federal broadband or telehealth programs?
Are there any eligible institutions in your community that could benefit from knowledge about telehealth programs and grants?
Is there widespread awareness of the Federal Emergency Broadband Benefit in your community?
Improving Your Community's Telehealth Capabilities

Now that you understand the problems many rural communities encounter as they work to implement telehealth, you are ready to strengthen your community's capacity for high-quality, sustainable telehealth systems. As you ideate solutions for your community, consider exploring methods for making change at the local level and possible strategies that fit within these levels. The chart below provides examples that address some of the weaknesses in current policies as discussed in this article.

Now It's Time to Use What You've Learned to Bring Telehealth to Your Community

Start by assessing the needs of your community.
Ask questions like:
- What kind of digital infrastructure does the community have?
- What level of digital health literacy does the community have?
- Who are the providers in the community?
- Are the providers using telehealth?
- Do the providers have the resources and knowledge to use telehealth?
Identify your local stakeholders and build connections.
Consider:
- Federal, state, and local government officials
- Local health care providers
- Information technology companies
- Churches, libraries, and other community institutions
- Community residents
Meet with stakeholders and brainstorm ideas.
Remember:
- Don't rule out ideas when you're brainstorming
- Make sure everyone has a voice
Assess each idea according to feasibility and your community priorities.
Consider:
- The results of your needs assessments
- The balance between the priorities of providers and community residents
- Available community funding
- Timeframe for implementation
- Resources required for initial investment
- Resources required for maintaining intervention if necessary
Decide which idea to implement first and get started! Remember:
- You don't need to fix every problem at one time
- Ensure you have the necessary resources to carry out your idea
Rural communities have unique needs, and the resource intensive nature of improving telehealth access in rural communities means every problem can’t be solved at once. Find the best place to get started for your community and get started.
Image Sources:
- "Landscape Sunset Field Bridge" by Pavel on Pexels
- "Brown Wheat Field During Sunset Photo" by Tim Hufner on Unsplash
Sources:
- Rural Health Information Hub. Rural Health Disparities. Available from: https://www.ruralhealthinfo.org/topics/rural-health-disparities.
- Rural Health Information Hub. Specific Rural Populations that May Benefit from Telehealth. Available from: https://www.ruralhealthinfo.org/toolkits/telehealth/1/benefits-for-specific-populations.
- Ellison, A. State-by-state breakdown of 130 rural hospital closures. 2020. Available from: https://www.beckershospitalreview.com/finance/state-by-state-breakdown-of-130-rural-hospital-closures.html.
- One in 10 Americans Use Telehealth, But Nearly 75% Lack Awareness or Access, J.D. Power Finds, in PRNewsWire. 2019, J.D. Power. Available from: One in 10 Americans Use Telehealth, But Nearly 75% Lack Awareness or Access, J.D. Power Finds (prnewswire.com)
- Perrin, A., Digital gap between rural and nonrural America persists. 2019. Available from Digital gap between rural and nonrural America persists Pew Research Center
- National Rural Health Association. About Rural Health Care. Available from: https://www.ruralhealthweb.org/about-nrha/about-rural-health-care.
- Rural Health Information Hub, Barriers to Telehealth in Rural Areas. Available from: Barriers to Telehealth in Rural Areas - RHIhub Toolkit (ruralhealthinfo.org)
- Schadelbauer, R., Anticipating Economic Returns of Rural Telehealth. 2017. Available from Microsoft Word - Report - Final Times Roman.docx (ntca.org)
- Rural Health Information Hub. Telehealth Use in Rural Healthcare. Available from: https://www.ruralhealthinfo.org/topics/telehealth.
- Weigel, G., et al., Opportunities and Barriers for Telemedicine in the U.S. During the COVID-19 Emergency and Beyond, in Kaiser Family Foundation. 2020. Available from: Opportunities and Barriers for Telemedicine in the U.S. During the COVID-19 Emergency and Beyond KFF
- HHS. Telehealth: Delivering Care Safely During COVID-19. Available from: https://www.hhs.gov/coronavirus/telehealth/index.html.
- Cooper, T. Rural Digital Opportunity Fund (RDOF) – Map, Auction and Analysis. 2021; Available from: https://broadbandnow.com/report/rural-digital-opportunity-fund/.
- USDA. Distance Learning & Telemedicine Grants. Available from: https://www.rd.usda.gov/programs-services/distance-learning-telemedicine-grants.
- FCC. Emergency Broadband Benefit. Available from: https://www.fcc.gov/broadbandbenefit.
- HHS and USDA, Rural Action Plan. 2020. Available from Department of Health and Human Services - Rural Action Plan - September 2020 (hhs.gov)
- Jaret, P. Attracting the next generation of physicians to rural medicine. 2020. Available from: https://www.aamc.org/news-insights/attracting-next-generation-physicians-rural-medicine.
- CDC. Rural Americans are dying more frequently from preventable causes than their urban counterparts. Available from: Rural Americans are dying more frequently from preventable causes than their urban counterparts | CDC Online Newsroom | CDC
- Simpson, A. Rural Hospitals Hang on as Pandemic Reaches Smaller Communities. 2020. Available from: Rural Hospitals Hang on as Pandemic Reaches Smaller Communities | The Pew Charitable Trusts (pewtrusts.org)
- Poon, L. There Are Far More Americans Without Broadband Access than Previously Thought. 2020. Available from: Where the U.S. Underestimates the Digital Divide - Bloomberg
